Lumbar puncture is the introduction of a hollow needle into the subarachnoid space of the lumbar portion of the spinal column to diagnose suspected infection and remove blood or pus. Cerebrospinal fluid (CSF) is completely replaced about three times a day. Although about 500 mL of CSF is formed every day, much of it is reabsorbed into the blood. There are about 120 to 150 mL of CSF in the system at any one time.
RATIONALE
● To determine or to rule out central nervous system infection;
● To determine the level of pressure in spinal column;
● To introduce drugs into the spinal canal (called an intrathecal injection).
INDICATIONS
Samples of CSF are taken for:
● Taking cell counts (a tiny number of white cells may normally be present);
● Measuring glucose and protein (also present in small quantities);
● Cytology, i.e. looking for abnormal cells;
● Immunoglobulin (antibody) studies;
● Bacterial or viral tests;
● Biochemical analysis.
CONTRAINDICATIONS
● Lumbar skin infection
● Platelet count less than 50,000/μL
● Degenerative joint disease
● Increased intracranial pressure
COMPLICATIONS
● Severe headache
● Meningitis from introducing bacteria into CSF
● Back or leg pain/paresthesia
● Accidental puncture of spinal cord
● Accidental puncture of aorta or vena cava
● Herniation of brain due to sudden decrease in pressure
PROCEDURE
Lumbar Puncture
Equipment
● Spinal tap tray
● Mask
● 22- to 23-gauge needle
● Syringe
● Manometer
● CSF specimen collection bottles
● Skin spray
● 1% lidocaine
● Povidone-iodine
● 22-gauge spinal needle
● Sterile gloves
● Fenestrated drape
● 2 × 2 gauze
● Tape
Procedure
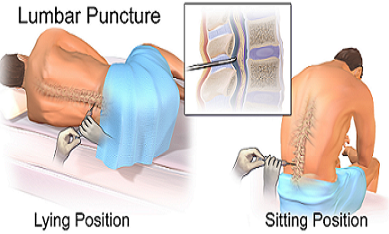
● Position client in tripod (fetal) or lateral recumbent (fetal/child/adult) position.
● Have client clasp hands on the knees.
● Draw a line across the back between the top of the iliac crests. Locate the interspace between either L4-5 or L5 S1 (preferred) (Fig. 29.1). Mark with barrel of syringe.
● Open the spinal tray.
● Apply mask.
● Put on sterile gloves.
● Cleanse the skin 6 inches around the interspace with povidone-iodine in a circular motion.
● Cleanse the same area with 70% alcohol.
● Draw up 3 mL of 1% lidocaine.
● Assemble the manometer with the three-way stopcock.
● Inject the lidocaine at the site, raising a wheal in the skin. Inject 0.5 mL of lidocaine into the posterior spinous region.
● Insert the spinal needle with stylet in place through the skin just below the palpated spinous process. Angle about 15 degrees cephalad.
● If you hit bone or the needle meets with resistance, withdraw the needle slightly and redirect.
● Advance the needle slowly.
● After the needle is inserted a few millimeters, withdraw the stylet to see whether CSF is present. You may hear a popping sound when the needle penetrates the dura.
● Advance the needle 1 to 2 mm farther.
● Remove the stylet.
● Attach the manometer to the hub of the inserted needle. Note the level of pressure on the manometer.
● Open the stopcock to allow the CSF to flow into the test tubes. CSF collection usually takes 5 to 10 seconds. Do not attempt to aspirate CSF with a syringe.
● If blood returns, remove needle and discard.
● Repeat procedure with fresh needle.
● Remeasure level of pressure. Do not withdraw CSF if pressure is significantly different.
● Label the tubes (See table below).
● When enough CSF has been obtained, replace the stylet and remove the needle.
● Spray the skin.
● Cover the insertion site with a 2 × 2 pressure dressing and leave in place for 2 hours.
● Send tubes to laboratory within 2 hours for analysis (See table below). Do not refrigerate the tubes.
Labeling Tubes
| TUBE NO | PURPOSE OF TEST |
|---|---|
| 1. Biochemistry | Glucose, protein |
| 2. Bacteriology | Varying shades of pink to coral red; Gram stain, culture (bacterial); Indicate whether the following are needed (Fungal culture, TB culture, Viral culture) |
| 3. Hematology | Cell count, differential |
| 4. Optional | VDRL,India ink (fungal), Cytology, Myelin basic protein, Oligoclonal bands |
TB, tuberculosis; VDRL, Venereal Disease Research Laboratory.
Normal Cerebrospinal Fluid
| TEST | NORMAL VALUE | INDICATION |
|---|---|---|
| Opening pressure | 50 to 200 mm H2O | No intracranial pressure, No obstruction |
| WBC glucose | <5/mm3 50% to 80% of serum glucose | No infection, No hypoglycemia or hyperglycemia |
| Protein | 15 to 45 mg/dL | No hemorrhage, No tumors, Nontraumatic tap |
| Color | Clear and colorless | No bacteria, WBCs, or bleeding |
| RBC | <20 | Nontraumatic tap |
WBC, white blood cell; RBC, red blood cell.
Abnormal Cerebrospinal Fluid Values
| TEST | NORMAL | ABNORMAL | INDICATION |
|---|---|---|---|
| Appearance | Clear | Cloudy, Bloody | Infection, Hemorrhage, obstruction, or traumatic tap |
| Appearance | Brown, yellow, orange | Elevated protein, RBC hemolysis present for ≥3 days | |
| Protein | 15 to 45 mg/dL | Increase | Tumors, trauma, hemorrhage, diabetes mellitus, polyneuritis, blood in CSF |
| Protein | Decrease | Rapid CSF production | |
| Gamma globulin | 3% to 12% | Increase | Multiple sclerosis, neurosyphilis, Guillain-Barré syndrome |
| Glucose | 50% to 80% | Increase | Systemic hyperglycemia |
| Glucose | Decrease | Systemic hypoglycemia, Bacterial or fungal infection, meningitis, mumps | |
| Cell count | 0 to 5 WBCs, No RBCs | Increase | Active disease, meningitis, tumor, abscess, infarction, multiple sclerosis |
| Cell count | RBCs present | Hemorrhage, traumatic tap | |
| VRDL | Nonreactive | Positive | Neurosyphilis |
| Chloride | 118 to 130 mEq | Decrease | Meningitis, TB |
| Gram stain | Negative | Gram-positive or -negative organisms | Bacterial meningitis |
RBC, red blood cell; CSF, cerebrospinal fluid; WBC, white blood cell; VDRL,Venereal Disease Research
Laboratory; TB, tuberculosis.
Nursing considerations
● Lumbar puncture is a strict aseptic technique requiring full sterile procedures.
● Encourage patients to drink well before and after the procedure.
● Positioned the patient carefully, laying on one side in a curled up position with the lumbar spine exposed (knees drawn up to the chest). Moving the patient’s back closer to the edge of the bed will make access to the lumbar spine easier. Support the patient in this position throughout the procedure.
● A small local sterile dressing is applied to the spinal site after removal of the needle.
● Headache is a common complaint following lumbar puncture. The patient should lay flat for 6-12 hours afterwards, as sitting up may make any headache worse.
● In myelograms, the patient’s head should be kept raised for up to 24 hours afterwards to prevent contrast medium in the spinal canal from entering the skull. This may caused seizures if it passes around the brain (Blows, 2002).
● Have the client avoid strenuous activity for first 24 hours after procedure.
Post Procedure Care
● Monitor vital signs and neurological status.
● Assess LP site for bleeding or CSF leak every 15 minutes for one hour. Maintain patient in supine position for 1 hour or as ordered.
● Assess for presence of headache and nausea. Administer analgesic and antiemetic as ordered.
● Report to physician of any significant changes in vital signs or neurological status, including pupillary changes, swelling, bleeding or CSF leak at LP site, tingling or loss of sensation/function of lower limbs, changes in bowel or bladder control, headache or nuchal pain or rigidity.
BIBLIOGRAPHY
● American Thoracic Society. Lumbar puncture; 2000. www.thoracic.org.
● Fischbach F. A manual of Laboratory and Diagnostic Tests. 6th ed. Philadelphia, PA: Lippincott; 2001.
● Intermed Communications, Inc. Diagnostics: An A-Z Guide to Laboratory Tests. Springhouse, PA: Intermed Communications, Inc; 2000.
● Neurology. Protocol for lumbar puncture; 2002. http://www.neuro.nwu.edu.
CLICK HERE for more resources on Laboratory and Diagnostics Test