Bronchoscopy
Description
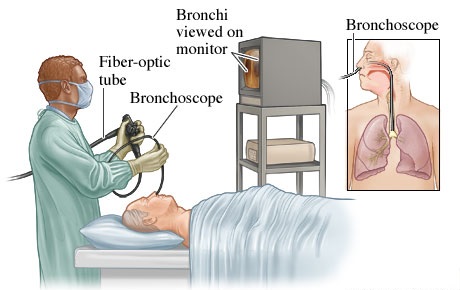
Bronchoscopy allows direct visualization of the larynx, trachea, and bronchi through a flexible fiberoptic bronchoscope or a rigid metal bronchoscope. A more recent approach is the use of virtual bronchoscopy.
Although a flexible fiberoptic bronchoscope allows a wider view and is used more commonly, the rigid metal bronchoscope is required to remove foreign objects, excise endobronchial lesions, and control massive hemoptysis. A brush, biopsy forceps, or catheter may be passed through the bronchoscope to obtain specimens for cytologic examination.
Bronchoscopy may require fluoroscopic guidance for distal evaluation of lesions for a transbronchial biopsy in alveolar areas. However, the usual bronchoscopy procedure is as follows:
• With the patient sitting upright or lying supine, a local anesthetic is sprayed into the patient’s throat.
• Once the anesthetic takes effect, a bronchoscope is introduced through the patient’s mouth or nose.
• When the scope is just above the vocal cords, about 3 to 4 mL of 2% to 4% lidocaine is flushed through the
scope’s inner channel to the vocal cords to anesthetize deeper areas.
• The practitioner inspects the anatomic structure of the trachea and bronchi, observes the color of the mucosal lining, and notes masses or inflamed areas.
• Tissue specimens may be obtained from a suspect area; a bronchial brush to obtain cells from the surface of a lesion, and a suction apparatus to remove foreign bodies or mucus plugs may be used. Broncho alveolar lavage may be performed to diagnose the infectious causes of infiltrates in an immunocompromised patient or to remove thickened secretions.
CLICK HERE for more resources on Laboratory & Diagnostic Test
Purpose
• To visually examine a tumor, an obstruction, secretions, bleeding, or a foreign body in the tracheobronchial tree
• To help diagnose bronchogenic carcinoma, TB, interstitial pulmonary disease, and fungal or parasitic pulmonary infection by obtaining a specimen for bacteriologic and cytologic examination
• To remove foreign bodies, malignant or benign tumors, mucus plugs, and excessive secretions from the tracheobronchial tree
Normal Findings
• Trachea consisting of smooth muscle containing C-shaped rings of cartilage at regular intervals and lined with ciliated mucosa
• Bronchi appearing structurally similar to the trachea; the right bronchus slightly larger and more vertical than
the left
• Smaller segmental bronchi branching off the main bronchi
Abnormal Findings
• Bronchial wall abnormalities, such as inflammation, swelling, protruding cartilage, ulceration, tumors, and mucous gland orifice or submucosal lymph node enlargement
• Endotracheal abnormalities, such as stenosis, compression, ectasia (dilation of tubular vessel), irregular bron chial branching, and abnormal bifurcation due to diverticulum
• Abnormal substances in the trachea or bronchi, such as blood, secretions, calculi, and foreign bodies
• Evidence of interstitial pulmonary disease, bronchogenic carcinoma, tuberculosis (TB), or other pulmonary infections
CLICK HERE for more resources on Fundamentals of Nursing
Nursing Implications
• Anticipate the need for additional testing, if indicated.
• Radiographic, bronchoscopic, and cytologic findings must be correlated with clinical signs and symptoms.
Interfering Factors
• Failure to place specimens in the appropriate containers
Precautions
• A patient with respiratory failure who can’t breathe adequately on his own should be placed on a ventilator before bronchoscopy.
Nursing Considerations
Before the Test
• Confirm the patient’s identity using two patient identifiers according to facility policy.
• Explain to the patient that bronchoscopy is used to examine the lower airways.
• Describe the procedure, including that it’s done in a darkened room. Tell him who will perform the test, and when and where it will occur.
• Explain to the patient that he’ll need to fast for 6 to 12 hours before the test and that he may receive an IV
sedative to help him relax.
• If the procedure isn’t being performed under general anesthesia, inform the patient that a local anesthetic will be sprayed into his nose and mouth to suppress the gag reflex. Warn him that the spray has an unpleasant taste and that he may experience discomfort during the procedure.
• Reassure the patient that his airway won’t be blocked during the procedure and that oxygen will be administered
through the bronchoscope.
• Make sure that the patient or a responsible family member has signed an informed consent form.
• Check the patient’s history for hypersensitivity to the anesthetic.
• Obtain the patient’s baseline vital signs.
• Administer the preoperative sedative.
• Have the patient remove his dentures, if appropriate, before he receives a sedative.
During the Test
• Place the patient in the supine position or have him sit upright in a chair.
• Tell the patient to remain relaxed with his arms at his sides and to breathe through his nose.
• Provide supplemental oxygen by nasal cannula, if necessary.
• Assist with tissue specimen collection, as indicated.
• After collection, place the specimens in their respective, properly labeled containers in accordance with laboratory and pathology guidelines, and send them to the laboratory at once.
CLICK HERE for more resources on Medical Surgical Nursing
After the Test
• Monitor the patient’s vital signs per facility policy, or at least every 15 minutes until the patient is stable and then every 30 minutes for 4 hours, every hour for the next 4 hours, and then every 4 hours for 24 hours. Immediately notify the practitioner of adverse reactions to the anesthetic or sedative.
• Place the conscious patient in semi-Fowler’s position; place the unconscious patient on his side with his head slightly elevated to prevent aspiration.
• Provide an emesis basin, and instruct the patient to spit out saliva rather than swallow it. Observe sputum for
blood, and report excessive bleeding immediately.
• Tell the patient who has had a biopsy to refrain from clearing his throat and coughing, which may dislodge the clot at the biopsy site and cause hemorrhaging.
• Immediately report subcutaneous crepitus around the patient’s face and neck, because this may indicate tracheal or bronchial perforation.
• Restrict food and fluids to avoid aspiration until the gag reflex returns (usually in 1–2 hours). The patient
may then resume his usual diet, beginning with sips of clear liquid or ice chips.
• Reassure the patient that hoarseness, loss of voice, and sore throat are temporary. Provide lozenges or a soothing liquid gargle to ease discomfort when his gag reflex returns.
Nursing Alert
Watch for, listen for, and immediately report symptoms of respiratory diffi culty resulting from laryngeal edema or laryngospasm, such as laryngeal stridor and dyspnea. Observe for signs and symptoms of hypoxemia, pneumothorax, bronchospasm, and bleeding.
Reference:
Brunner & Suddarth’s (2010). Handbook of laboratory and Diagnostic Test. New York: Lippincott Williams & Wilkins