Normal Findings
- Normal knee consisting of a diarthrodial joint surrounded by muscles, ligaments, cartilage, and tendons, and lined with a synovial
membrane - In children, smooth and opaque menisci, with thick outer edges attached to the joint capsule and unattached inner edges lying snugly
against the condylar surfaces - Articular cartilage that’s smooth and white
- Ligaments and tendons that are cablelike and silvery
- Synovium that’s smooth and marked by a fine vascular network
Abnormal Findings
- Meniscal disease, such as a torn medial or lateral meniscus or other meniscal injuries
- Patellar disease (chondromalacia, dislocation, subluxation, parapatellar synovitis, or fracture)
- Condylar disease (degenerative articular cartilage, osteochondritis dissecans, and loose bodies)
- Extrasynovial disease (torn anterior cruciate or tibial collateral ligaments, Baker’s cyst, and ganglionic cyst)
- Synovial disease (synovitis, rheumatoid and degenerative arthritis, and foreign bodies associated with gout, pseudogout, and osteochondromatosis)
Nursing Implications
- Report abnormal findings to the practitioner.
- Educate the patient about his diagnosis and possible treatment options.
- Depending on test findings, appropriate treatment or surgery can follow arthro scopy. If arthroscopic surgery can’t be performed, arthrotomy is the procedure of choice.
Purpose
- To detect and diagnose meniscal, patellar, condylar, extrasynovial, and synovial diseases
- To monitor disease progression
- To perform joint surgery
- To monitor the effectiveness of therapy
Description
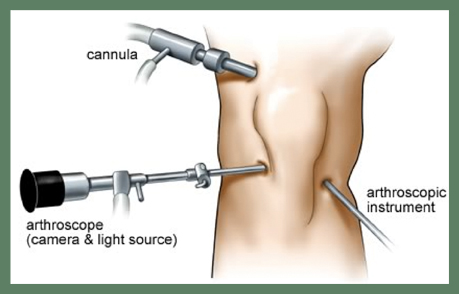
Arthroscopy is the visual examination of the interior of a joint (most commonly a major joint, such as a shoulder, hip, or knee) with a specially designed fiberoptic endoscope that’s inserted through a cannula in the joint cavity. It usually follows and confirms a diagnosis made through physical examination, radiography, and arthrography. Arthroscopy may be performed under local anesthesia, but it’s usually performed under a spinal or general anesthesia, particularly when surgery is anticipated. A camera may be attached to the arthroscope to photograph areas for later study.
Arthroscopic techniques vary depending on the surgeon and the type of arthroscope used. The procedure typically proceeds as follows:
- The patient’s leg is elevated and wrapped with an elastic bandage to drain as much blood from the leg as possible, or a mixture of lidocaine with epinephrine and normal saline solution is instilled into the patient’s knee to distend the knee and reduce bleeding.
- The local anesthetic is administered, a small incision is made, and a cannula is passed through the incision and positioned in the joint cavity.
- The arthroscope is inserted, and the knee structures are visually examined and photographed for further study.
- After visual examination, a synovial biopsy or appropriate surgery is performed, as indicated.
- When the examination is completed, the arthroscope is removed, the joint is irrigated, the cannula is removed, and an adhesive strip and compression dressing are applied over the incision site.
Precautions
- Arthroscopy is contraindicated in the patient with fibrous ankylosis with flexion of less than 50 degrees.
- Arthroscopy is contraindicated when the patient has local skin or wound infections with a risk of subsequent joint involvement.
Nursing Considerations
Before the Test
- Explain to the patient that arthroscopy is used to examine the interior of the joint, to evaluate joint disease, or to monitor his response to therapy, as appropriate.
- Describe the procedure to the patient and answer his questions.
- If surgery or another treatment is anticipated, explain that this may be accomplished during arthroscopy.
- Instruct the patient to fast after midnight before the procedure.
- Inform the patient who will perform the procedure, and when and where it will be done.
- If local anesthesia is to be used, advise the patient that he may experience slight discomfort from the local anesthetic injection and the tourniquet pressure on his leg.
- Also prepare him to expect to feel a thumping sensation as the cannula is inserted in the joint capsule.
- Make sure that the patient or a responsible family member has signed an informed consent form.
- Check the patient’s history for hypersensitivity to the anesthetic.
- Prepare the surgical site by shaving the area 5” (12.7 cm) above and below the joint, and administering a sedative, as ordered.
- Position the patient, and drape him according to facility policy.
After the Test
- Observe the patient for fever, swelling, increased pain, and localized inflammation at the incision site. If the patient reports discomfort, provide an analgesic, as ordered.
- Monitor the patient’s circulation and sensation in his leg.
- Advise the patient to elevate the leg and apply ice for the first 24 hours.
- Instruct the patient to report fever, bleeding, drainage, or increased swelling or pain in the joint.
- Advise the patient to bear only partial weight, using crutches, a walker, or a cane for 48 hours.
- If an immobilizer is ordered, teach the patient how to apply it.
- Tell the patient that showering is permitted after 48 hours, but a tub bath should be avoided until after the postoperative visit.
- Tell the patient that he may resume his usual diet, as ordered.
Reference:
Brunner & Suddarth’s (2010). Handbook of laboratory and Diagnostic Test. New York: Lippincott Williams & Wilkins